FIP-EquityRx Collection 2020: Inequities unmasked

Dear Readers,
Welcome to the FIP-EquityRx Collection 2020 “Inequities unmasked”, the second FIP-EquityRx Collection!
We launched the first FIP-EquityRx Collection in 2019 with the theme “Inclusion for all, equity for all” which was the inaugural ‘FIP Collection’ publication. Since then we have also published a Transforming Vaccination Globally & Regionally Collection, which captures the key outcomes of the 2020 digital programme of the same name. The FIP Pharmacy Education Journal also published a timely COVID-19 Special Collection which reports on the global responses to teaching, learning and delivery in pharmacy education during the pandemic.
Both FIP-EquityRx Collections share the same function as compilations of global evidence, policy initiatives, opinion pieces, and seasonal features focusing on a selected FIP & pharmacy priority programme of work (in this case equity). However, the two Collections differ in two very distinct and important ways:
- The first edition was pre-COVID-19 “era”, the global event that upended our lives as we knew it before.
- This edition of the Collection is an easily accessible digital version, published on a new FIP-EquityRx resource site, with an imperative that this FIP-EquityRx Collection focussed on the inequities ‘unmasked’ by the pandemic.
Some of those inequities are long standing ones that have not only risen to the fore but also in most cases been worsened by the pandemic; others, however, are an unfortunate direct consequence of COVID-19. Another important milestone that differentiates the two Collections was the launch of the FIP Development Goals (FIP DGs) in September 2020.
The FIP DGs build on the 2016 Pharmaceutical Workforce Development Goals, expanding their scope to 21 goals that address goals across not only workforce & education, but also practice and science. This is reflected in FIP DG 10 “Equity and equality”. The evolution of DG 10, the FIP-EquityRx programme of work, what equity means for pharmacy are explored in the next two sections of the Collection. The FIP View provides a comprehensive review of FIP-EquityRx while the Leading Editorial features a digital video message from one of our FIP Global Leads on DG10, Vibhuti Arya who emphasises why equity matters to us all now more than ever.
This is followed by a special feature on vaccine equity where we highlight our 2020 work to transform vaccination in pharmacy and identify mechanisms to address vaccination inequities, using the FIP DGs as an operational framework. We also present to you a new FIP Statement of Principle on vaccine equity for pharmacy teams, which FIP has published with this Collection.
A story of pharmacists supporting patients in lockdown with access to essential medicines is shared in ‘’Medicines Access in Isolation.” This story describes how patients were able to access medicine and opioid replacement therapy, with the support of pharmacy during the strict lockdown. This is an example of the essential role that pharmacy plays in providing access to care everywhere around the world.
“The Shadow Pandemic” refers to the global increase in domestic violence amid the COVID-19 health crisis. A dedicated section in our Collection illustrates this shadow pandemic with examples from around the world – specifically highlighting the increase in gender-based violence against women. Importantly, the role of pharmacy in supporting those victims and patients is also discussed.
A number of opinion pieces on safety & equity in the workplace are featured in this issue’s “Exposed” section. Carlene Ngoma, FIP’s Global Lead on FIP DG 10 Equity and equality, shares collected experiences in regards to two important issues in the workplace, especially common for women: dealing with sexual harassment and navigating maternity and paternity leave for new parents. Kay Dunkley sheds light on the abuse and violence facing health workers, including pharmacy teams.
This Collection’s “Evidence Room” shares the results of a research study that exemplifies the how disproportionate health inequities are, and how COVID-19 has merely highlighted them. The researchers demonstrate that either due to underlying co-morbidities, systemically mediated healthcare inequities, or a combination of these factors, African Americans are at much higher risk of COVID-19-related mortality compared to all other ethnicities.
“The Unfair Rollout” is a personal account by Elizabeth Ridgway, a young pharmacist on the frontline and our FIP-EquityRx Programme Coordinator, who reports on her first-hand experience of how vaccine rollouts, while intended to protect and serve the most vulnerable communities, sometimes does not allow for vaccines to reach them at all. This is another piece that sheds light on how pharmacists can and do reduce the access gap to life-saving vaccines.
In our 2019 FIP-EquityRx Collection, we presented examples of transformative policies & initiatives from around the globe; a national case example from Pakistan was featured. More than a year onwards, those efforts in Pakistan have blossomed into a national equity hub, an effort co-led by Nadia Bukhari, FIP Global Lead for 10 Equity & equality. Find out more in “FIP-EquityRx in Action”.
In “FIPWiSE & the Pandemic”, the FIP initiative for Women in Education and Science describes its history – including past, current and future activities, especially highlighting how women in science and education are at the forefront of the fight against COVID-19.
As we pen this Editorial, we are very much aware we are still – unfortunately – living in the midst of the pandemic.
We also are aware that the fallout from it, especially in regard to its impact on health equity are likely to remain for years and even decades to come… and inequities will continue to emerge, including across our profession, our societies and our communities. FIP-EquityRx will continue to bring to the forefront these issues affecting workforce & education, practice and science, while FIP will continue to support each of you and shine a light on practice and evidence along the way.
While we strived to cover as many of these angles as possible in this Collection, one Collection will never be complete. We encourage you to keep an eye out for new activities & resources at the new equityrx.fip.org site which collates al ofl our equity work: past, present and future.
We hope you enjoy this Collection and if you have not joined us live in its digital launch event, you can play it back here.
Happy reading!
We hope you enjoy this Collection and if you have not joined us live in its digital launch event, you can play it back
here.
Dr Catherine Duggan, Chief Executive Officer, FIP (The Netherlands)
Dr Lina Bader, FIP Lead for FIP-EquityRx & FIP Lead for Workforce Transformation and Development, FIP (Saudi Arabia)
Note from the Editors: Our Leading Editorial this year is a video message from one of our FIP Global Leads on DG10, Vibhuti Arya who emphasises why equity matters to us all now more than ever.
Authors: Lina Bader, FIP Lead for FIP-EquityRx & FIP Lead for Workforce Transformation and Development, FIP (Saudi Arabia) & Catherine Duggan, Chief Executive Officer, FIP (The Netherlands)

What is FIP-EquityRx?
The FIP Development Goals are set to transform global pharmacy by providing a systematic and integrated framework that can support the transformation of pharmacy practice, science and workforce & education. Of the 21 Goals, many are relevant to our profession, many are relevant to our patients but the FIP Development Goal 10 is one that impacts us all. The past year has shown we can and must not take Equity and Equality for granted.
The Equity & Equality Development Goal calls for clear strategies to address inequalities in the pharmaceutical workforce, widen access and equity of pharmaceutical care services & access, as well equity in global capacity in pharmaceutical sciences development. FIP-EquityRx – FIP’s programme on Equity & Equality in pharmacy – is driving FIP implementation of DG 10’s.
FIP Development Goal 10 builds on the Pharmaceutical Workforce Development Goal (PWDG) 10 “Gender and diversity balances” and expands the scope of the goal to include practice and science Elements and mechanisms for each such that the programme of work covers: equity & equality in pharmaceutical workforce & education; equity & equality in pharmaceutical practice; and equity & equality in pharmaceutical science.
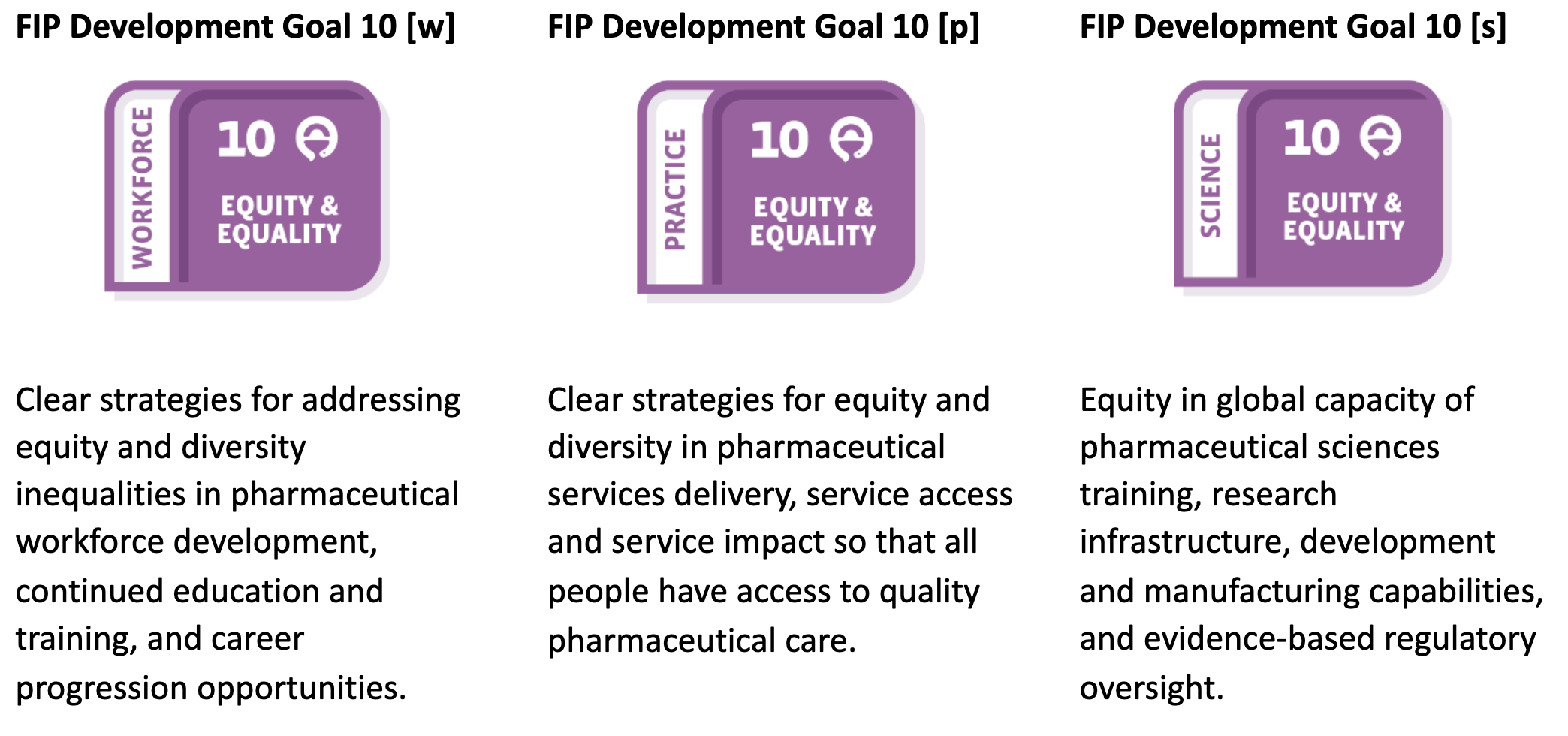
In 2018, FIP-EquityRx became the overarching label and unifying theme for FIP’s initiatives and work on gender and diversity. These initiatives focused on empowering women both within and beyond the workforce through promoting equity in the pharmacy workforce, championing women in science and academia and empowering women as informal caregivers. In 2019, through the FIP-EquityRx Collection 2019, FIP announced the expansion of the scope of its equity & equality programme to beyond gender & diversity balances — extending to equity in access to care and all that this encompasses. Since the launch of FIP Development Goal 10: Equity & Equality in 2020, this scope expansion became an even stronger imperative to support the equitable access to health care for all individuals, regardless of the following social, demographic and health identifiers & their intersectionality:
FIP-EquityRx programme of work & selected activities 2020
Operating under the motto ‘Pharmacy leaving no one behind’, FIP-EquityRx is a large programme encompassing many unique areas of work, all of which come together to support equity and equality for all. In addition to growing our global partnerships, FIP-EquityRx delivers publications, tools, frameworks, digital events to support our members transform the agenda nationally. To support our members navigate through all of these benefits and activities, we have developed a new site full of resources dedication to FIP-EquityRx and DG10. It includes information about: our areas of work including workforce & education, practice and science; our global partnerships; events; publications and much more.
The site presents a comprehensive overview of our work, and this Collection highlights many of our 2020 activities and areas of focus (summarised in our Editorial). Below we spotlight other key 2020 activities you should know about and provide a glimpse of our 2021 plans and priorities.
A Workforce Reference Guide for equity and equality
FIP has a team of Global Leads on DG10 (through the Workforce Development Hub). Our Global Leads are dedicated volunteers whose mission is to support our members with the implementation of this goal through tools, frameworks and activities. They have recently published a Workforce Reference Guide for DG10. The digital Guide includes all information, evidence and expertise from FIP to support our members with measuring progress, evaluation, implementation and transformation processes with regards to the workforce elements of the Goal. You may access the Guide, find out more about those Leads, their outputs and ongoing projects here.
Digital events and features
A list of events delivered by FIP that address equity and equality in pharmacy from a number of angles and perspectives can be found here. Below we summarise a high-level digital event we held in September 2020 which captures and describes the evolution of FIP-EquityRx. Here’s a summary of the key outcomes:
- What is FIP Development Goal 10 and how it came to be? How will FIP-EquityRx drive this Goal? FIP’s Catherine Duggan & Lina Bader showcased the birth of FIP DG10… and our plans to tackle global priorities through FIP-EquityRx.
- How FIP DG 10 fits within the global quest for equity in health, women in health and access to quality care? We heard from Roopa Dhatt (Executive Director, Women in Global Health) on what more should pharmacy do. With Roopa, we announced our commitment to support the mission, vision, values and goals of the Women in Global Health COVID 50/50 campaign.
- What is the impact of inequities to access to medicines & pharmaceutical care on lives and nations? Through a regional lens, Adi Nuseirat (Technical Officer, World Health Organization) showed us the realities in the Eastern Mediterranean region..
- Why we need equity in pharmacy now! FIP’s ex-President Carmen Peña called on all of us to amp up the action…
- What does equity in pharmacy (workforce, practice and science) REALLY MEAN? We explored this question & more through a virtual roundtable with panelists from around the world including Claire Thompson, Nilhan Uzman, Nadia Bukhari, Vibhuti Arya, and Shane Desselle, Angie Lim Hui Li, Isaac Nii Ofoli Anang, Sherly Meilianti & many more.
FIP-EquityRx will be launching a ‘Commitment to Equity & Equality’, which will serve as an additional roadmap for committed & concerted action towards equity in pharmacy and support driving both the contribution of pharmacy towards a better and more inclusive world for all, as well as the FIP-EquityRx programme of work and its impact. We will welcome the new 2021 year with the second FIP-EquityRx Collection “Inequities unmasked” will focus on inequities and inequalities that the pandemic has exposed.
A Statement of Principle on equity during COVID-19
In May 2020, FIP also issued a Statement of Principle on the impact of the COVID-19 pandemic on health equity, and vulnerable patients and populations. FIP recognises that the impact of COVID-19 is closely linked to social determinants and will lead to increased vulnerability across communities, especially where there are underlying and existing problems. Addressing inequities and inequalities is more urgent than ever as the world battles a deadly pandemic. Recognising and identifying the most vulnerable patients and populations to COVID-19 is critical and urgent. It requires particular and specific protective strategies from governments and other stakeholders.
Pharmacy plays an important role in addressing and alleviating these inequities, and in serving vulnerable patients and populations during this pandemic. In particular, this statement focuses on various vulnerable population groups, such as women and children who suffer from violence during the COVID-19 pandemic; marginalised, displaced and underserved communities such as ethnic minorities, refugees and migrants, and people living in situations of informal economy; people living in countries with fragile and under-resourced health systems, with insufficient health workforce capacity, infrastructure or equipment; patients with underlying conditions including non-communicable diseases, which are in themselves a factor contributing to increased vulnerability to COVID-19; and older adults.
In this statement, FIP and pharmacists across the globe reaffirm their commitment to serve patients and communities in all settings of practice ― community, hospital, clinical biology and others ― throughout these challenging times of pandemic, and to promote equity in health protection and access to care across all people and especially the most vulnerable groups, leaving no-one behind.
The year ahead
In 2021, we continue activities that are primarily aimed at supporting our members with implementation. Key to this will be indicators and metrics that can help members measure and monitor progress against the Goals. Indicators for all 21 Development Goals, including DG 10, will be developed in 2021. These will support the existing Goal mechanisms which lay out tools and structures to support the process of transformation.
This year we will also follow through with announcing a global Commitment to Equity & Equality which describes a roadmap for Development Goal 10. We’re ensuring a consensus-based approach to developing this Commitment, and are therefore working with members from around the world to complete and a Commitment which truly reflects the wide scope of equity in pharmacy. The latest draft is currently being updated to reflect all elements of the widened Goal.
COVID-19 is here to stay (at least this year) and its effects on health inequities will continue for longer than we wish for. FIP-EquityRx will therefore continue to address these issues and challenges, often in a way that intersects with other Goals as well. Vaccine equity and access to services during the pandemic will remain a priority area of work. Assessing neds for development on a national and regional level will also guide us in identifying our member’s priorities and result in regional roadmaps that lay out the needs across all 21 Goals and Goal 10.
We will of course continue our other running activities and deliver more events, publications (including a 2021 Collection), our FIP-EquityRx Blogs and initiate needs-based projects. We invite our members to use our website to keep informed of these activities.
For any query related to FIP-EquityRx including requests for information or suggestions and ideas, please email lina@fip.org.
Contributors: Catherine Duggan, Chief Executive Officer, FIP (The Netherlands), Lina Bader, FIP Lead for FIP-EquityRx & FIP Lead for Workforce Transformation and Development, FIP (Saudi Arabia), Carlene Ngoma, Programme Coordinator Transforming Vaccination Globally & Regionally, FIP (Australia), Farah Aqqad, Project Coordinator Transforming Vaccination Globally & Regionally, FIP (Jordan) and Gonçalo Sousa Pinto, Programme Advisor Transforming Vaccination Globally & Regionally, FIP (Spain).

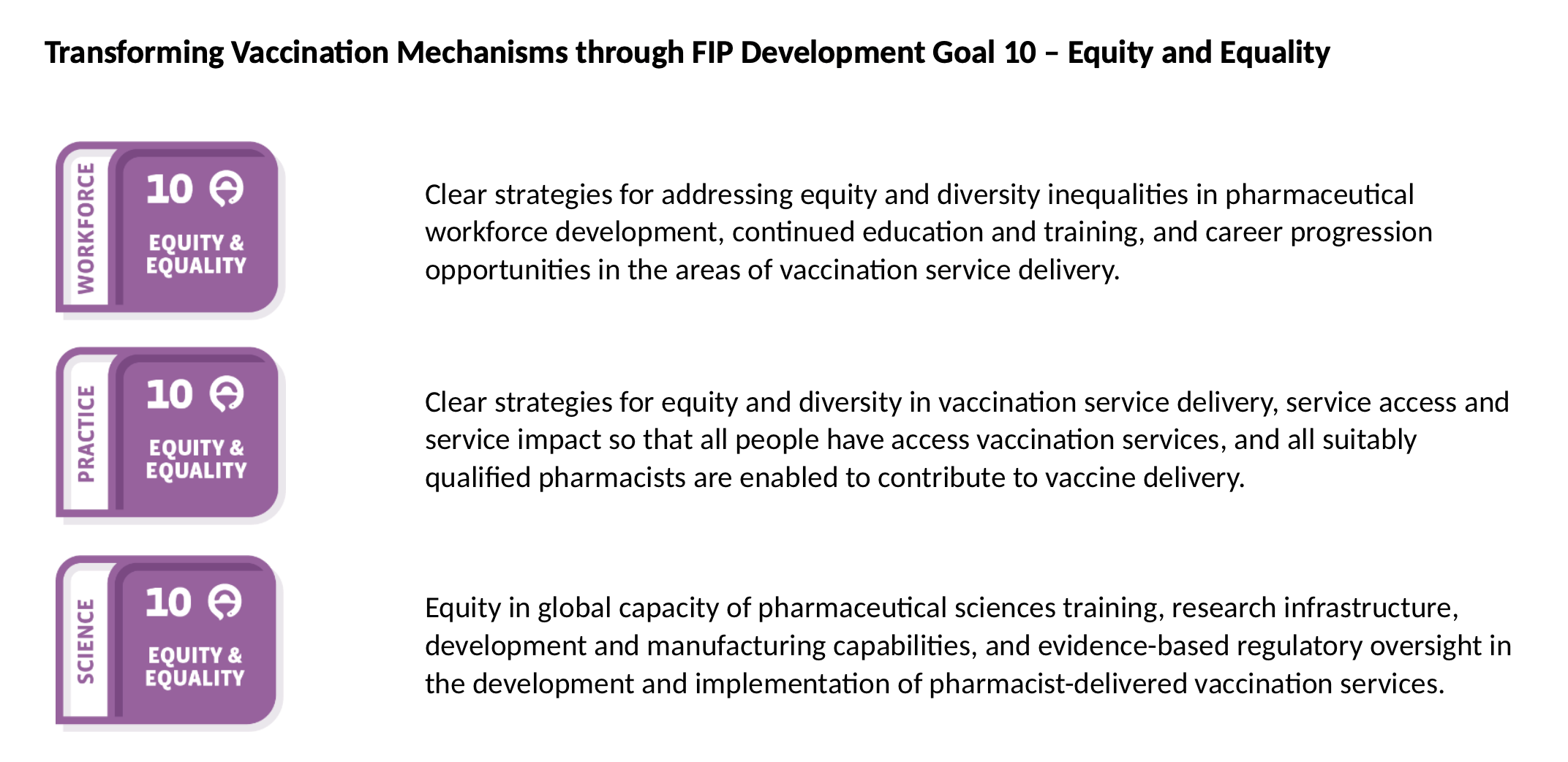
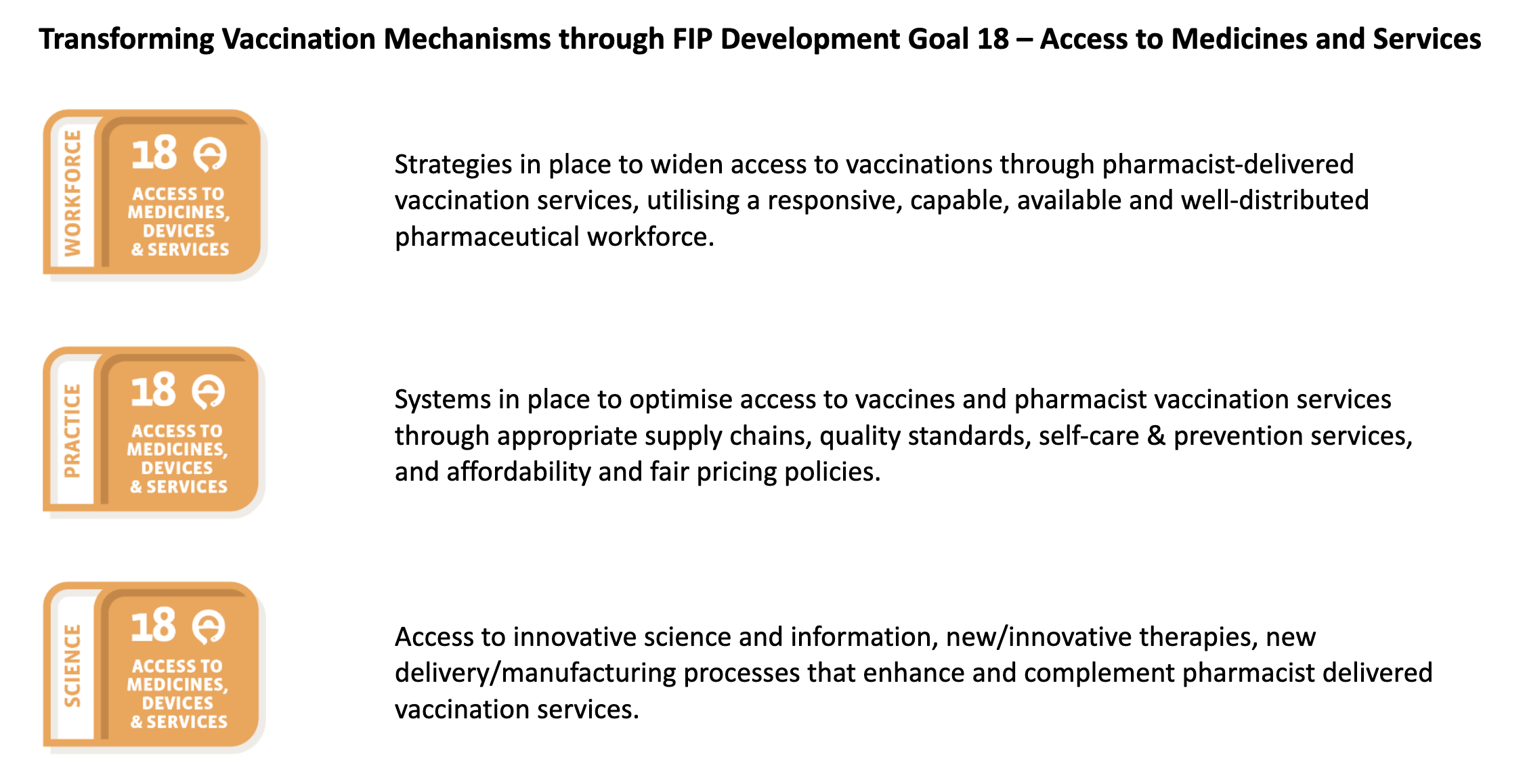
The FIP “Transforming Vaccination Globally and Regionally” programme delivered in 2020 was the first FIP digital transformation programme involving a three-part series of 24 digital events, culminating in a Global Summit and the FIP Commitment to Action on Improving Vaccination Coverage Through Pharmacies.
The second series in the programme consisted of 8 events that focused on the FIP Development Goals (FIP DGs) from the perspective of vaccination to identify actions to transform vaccination globally and regionally. The FIP DGs that were discussed include: FIP DG 10 equity and equality; FIP DG18 Access to Medicines & Services focusing on access to vaccination by all to improve health globally; FIP DG 13 Policy Development; FIP DG 19 Patient Safety; FIP DG 4 Advanced & Specialist Development, FIP DG 7 Advancing Integrated Services, FIP DG 16 Communicable Diseases; and FIP DG 17 Antimicrobial Stewardship. Series 2 of the Transforming Vaccination Globally and Regionally Programme was about Action. We took the global needs that were identified in series 1 and discussed the Actions that we need to take to address the Goals.
Episode 2.6 was titled “The Role of Pharmacist Vaccinators in Improving Access to and Equity in Healthcare Outcomes” and is aligned with FIP DG 10: Equity and equality and FIP DG 18: Access to medicines and services. Attendees discussed the role of pharmacists in ensuring that vaccinations are widely and easily accessible by all people in all areas of the world, and the expertise of pharmacists in delivering the logistics and services needed to increase vaccination rates. The session was moderated by Catherine Duggan FIP CEO (The Netherlands). Speakers included Jane Barratt, Secretary General, International Federation on Ageing (Canada) and Alexandra (Ali) Ruth, Doctoral Student, Johns Hopkins Bloomberg School of Public Health (USA).
The following tables summarise the outcomes Event 2.6 which has identified key mechanisms across the two Goals that can support the transformation of vaccination in pharmacy and can serve as an action plan that could be adopted and adapted by regions and countries worldwide.
You can watch the event recording here or download event slides.
FIP’s 2020 “Commitment to Action on Improving Vaccination Coverage Through Pharmacies” highlights actions that are urgently needed to ensure equitable access to vaccines and vaccination services for all people around the world. The commitment was during the first FIP Virtual Global Summit on transforming vaccination in pharmacy, and is the key outcome of FIP’s “Transforming vaccination globally and regionally” digital programme. FIP is also committed to supporting pharmacists and pharmacy workers with the most up-to-date intelligence on COVID-19 vaccines.
Concurrent with this Collection, FIP will launch a Statement of Principle which further supports the declaration and, in particular, calls for the acceleration of vaccine access for pharmacy teams on the frontline. We believe that ensuring early access of the pharmacy workforce to safe and effective COVID-19 vaccines will contribute to accelerating access to vaccines for all, as well as the continuity of treatments and other essential services, medical products and medical devices provided by pharmacy teams. Our statement highlights the critical role that pharmacy teams can play in immunising populations and contributing to improving vaccination coverage through, for example, evidence-based counselling. It also reaffirms the commitment of our profession across the globe to widening access to pharmaceutical services, particularly vaccination-related services, to ensure vaccine equity for all.
The Statement can be viewed here.
How people were able to access medicine and opioid replacement therapy during the strict lockdown with little notice – an account from Victoria, Australia
Author: Sheshtyn Paola MPH, Journalist, Australian Journal of Pharmacy (Australia).

On 4 July 2020, nine public housing towers in Melbourne, Australia, went into “hard lockdown”. This meant 3000 residents would be unable to leave their units for at least five days. The state government explained their rationale: these high-density towers were linked to some recent COVID-19 cases,1,2 and they were also home to some of the most vulnerable in the community. “This is about protection,” said Victorian Premier Dan Andrews. “We cannot have a cohort of people, many of whom … are in poor health to start with. We have to do everything we can to contain the virus.”3
While the government said it would provide support and essential items, stories quickly started flowing about difficulties faced by tower residents. Some reported challenges accessing food, getting scripts filled or receiving medication attention.4,5 One woman told HuffPost Australia she went the entire quarantine period without her prescription medication for a migraine condition.5
The Pharmaceutical Society of Australia (PSA) said pharmacists practising at nearby community pharmacies reported significant difficulties in providing medicines and care to people in the towers. 6 While local pharmacies were available to provide 24/7 care and medicine supplies throughout the tower lockdowns, they were not sufficiently utilised, explained PSA Victorian President John Jackson.7 Instead, some medicine supply ended up being centrally coordinated through the Royal Melbourne Hospital.
Brunswick pharmacist Angelo Pricolo confirmed the state health department reached out to the Pharmacy Guild about arranging access to opioid replacement therapy for affected residents.8 “Dosing methadone and buprenorphine for opioid replacement therapy is a bit tricky compared to dispensing most drugs, lots of mechanisms are in place to make sure patients are kept safe,” said Mr Pricolo. “Everyone was trying to devise a system that would be the easiest, quickest and least likely to fail in ensuring that all patients got their correct doses on time.
“In the end it was decided to work with the individual pharmacies that these patients had been attending. This meant all of their details were already recorded and also their dispensing history was readily available. From what I can gather, Royal Melbourne Hospital did pick up the slack but the preference was for local engaged pharmacy to continue servicing unless this was not possible…this was the case with opioid replacement therapy anyway. [Patients] definitely did not go without!”
Local pharmacists went above and beyond to support their patients. Dimitra Tsucalas from Ascot Vale Pharmacy confirmed she was able to organise medicines for her pharmacotherapy clients. “It all happened so suddenly,” she said of the lockdown. “Our patients called us the night before to warn us, so we could put things in place for the next day.” After trying to confirm what was going on with the police, and then with the coronavirus line, she eventually got the addresses of which towers were down. “We pulled a list of all of our pharmacotherapy patients, of who was where, got their phone numbers. The next morning I went in early before my shift and I rang them all and said, ‘I’m coming around to drop off your medication today.’ So I did a whole week’s supply, some were due for their dose that day, some were due on Monday.
“There was one patient I couldn’t get in touch with. I indicated who I was at the door to the police and they rang them and they came down. There was a pregnant lady who I delivered to that night. I also did two deliveries of non-pharmacotherapy [medicine] that Sunday as well, there was a young boy who had diabetes,” said Ms Tsucalas.
“We continued to cover pharmacotherapy until the next week. A system was then set up through cohealth based in Kensington, they coordinated deliveries by sending employees to our pharmacy to collect orders and take them back to the towers. It may not have been as efficient as us supplying directly. There would be specific times they would be delivering during the day. If we missed out on their cut off, it would’ve been complicated. I imagine if Royal Melbourne took over delivery of medications it would have been for new patients or new requests.
“I did have requests from one or two patients who didn’t have food. One of our patients, the pregnant lady, was quite scared so I tried to reassure her when I delivered her medication. I also kept in touch with our other clients and sent them notes and texts encouraging them,” she said.
References:
- https://theconversation.com/nine-melbourne-tower-blocks-put-into-hard-lockdown-what-does-it-mean-and-will-it-work-142033
- https://www.premier.vic.gov.au/statement-minister-housing
- Daniel Andrews Press Conference, 5/7/20. https://www.facebook.com/134712696593275/videos/312229309953082
- https://www.theage.com.au/national/victoria/shortages-of-food-medicine-and-trust-stories-from-lockdown-paint-a-picture-of-chaos-20200710-p55ard.html
- https://www.huffingtonpost.com.au/entry/prescription-medication-melbourne-hard-lockdown_au_5f0d087cc5b648c301ee86ce?guccounter=1
- https://www.psa.org.au/wp-content/uploads/2020/07/31-July-2020-PSA-COVID-19-Victorian-Submission.pdf
- PSA press release, 31/07/20.
- Email from A Pricolo to S Paola, 26/8/20.
Looking out for signs of abuse and mental health issues in patients or colleagues
Author: Sheshtyn Paola MPH, Journalist, Australian Journal of Pharmacy (Australia).

It is what experts are calling the ‘shadow pandemic’ – the rise in domestic violence experienced by women and girls as a secondary effect of COVID-19. A survey conducted by the Australian Institute of Criminology revealed a high rate of domestic violence experienced by women during the initial stages of the pandemic.1 For a third of women surveyed, it was the first time their partner had been violent. Others said violence was getting worse. “Confinement is fostering the tension and strain created by security, health, and money worries,” says Phumzile Mlambo-Ngcuka, Executive Director of UN Women.2 “It’s a perfect storm for controlling, violent behaviour behind closed doors.”
Pharmacists working on the frontline may be faced with the task of aiding patients experiencing violence, and may even observe signs and signals among colleagues. According to pharmacist and counsellor Helen Lowy, observable signs of trauma that can indicate domestic violence present in a range of ways. For example, there can be physical signs such as cuts and bruises; psychological signs including anxiety or depression; difficulties in accessing finances; or feelings of worthlessness, anger or shame, withdrawal and lack of engagement.
Ms Lowy says creating a safe environment includes assessing whether there is an immediate risk of threat and weighing this up against the likelihood of harm if immediate action is not taken. “If there is an immediate risk of threat, contact the police or ambulance or contact another emergency or crisis service for assistance,” she explains. “Otherwise, ensure that the person can speak in a secure, private space and consider whether it may be necessary to arrange care for children accompanying the adult. Do not ask questions in front of a suspected perpetrator.”
The pandemic has also had widespread psychological impacts, with higher levels of anxiety, depression, anger, confusion and loneliness across communities. According to the Black Dog Institute, people with pre-existing mental health problems, healthcare workers, those placed in quarantine and the unemployed or casual workers are at increased risk of distress during a disease outbreak.3
Pharmacists are not immune from the impacts of COVID-19. There was an 88% increase in calls from distressed Australian pharmacists over the most acute six-week period of the pandemic, Kay Dunkley, Executive Officer at the Pharmacists’ Support Service, told the Australian Journal of Pharmacy.4 The most common reason for calling related to COVID-19 was stress and anxiety. Pharmacists need to be kind to themselves during this time, says Ms Lowy. Some of her suggestions for mental wellbeing include unplugging from media; making time for exercise, nutrition and sleep; and practising mindfulness.5
Mental Health First Aid (MHFA) is crucial during this time, especially among pharmacists who are widely available healthcare professionals. “Learning how to spot the signs and symptoms of a mental health issue, and how to approach the person, and where to recommend they go for professional help are useful tools in the pharmacy environment – but also life in general,” says MHFA instructor Jan Decomps.6 Behavioural signs of a burgeoning mental health issue include excessive fear or worry; indecisiveness; erratic behaviour; withdrawal or avoidance of others; reduced participation in activities; and dishevelled appearance.
References:
- https://www.aic.gov.au/media-centre/news/shining-light-shadow-pandemic-new-report-reveals-high-rate-domestic-violence-experienced-australian-women-during-covid-19#:~:text=The%20Australian%20Institute%20of%20Criminology,of%20the%20COVID%2D19%20pandemic.&text=Half%20of%20those%20women%20with,increased%20in%20frequency%20or%20severity.
- https://www.unwomen.org/en/news/stories/2020/4/statement-ed-phumzile-violence-against-women-during-pandemic
- http://www.blackdoginstitute.org.au/wp-content/uploads/2020/04/20200319_covid19-evidence-and-reccomendations.pdf
- https://ajp.com.au/news/there-is-still-a-higher-than-normal-level-of-anxiety-in-pharmacy/
- https://ajp.com.au/news/be-kind-to-yourselves-at-this-time/
- https://ajp.com.au/news/a-compassionate-conversation/
Gender-based violence & the role of pharmacy
Author: Kay Dunkley, Executive Officer, Pharmacists’ Support Service (Australia)

According to the UN, for every three months the lockdown continues globally, an extra 15 million gender-based violence cases will occur. Prior to coronavirus there were already considerations and actions in place to address attitudes towards gender-based violence and gender equality; including gender pay gaps, the #MeToo movement, and addressing lack of female representation in leadership and representation bodies.
Some of the goals and actions to address these issues have been put on hold in order to address the increased number of women and girls at risk of gender-based violence, poverty and mental health challenges during the lockdown period.
As a result of the pandemic, a number of girls are leaving education for marriage due to economic hardship in certain countries. Girls may also be affected by parents and caregivers being locked down at home, unable to work, putting additional stress on these households and putting girls at further risk of harm. Where schools have been closed, girls miss out on life skills, information and services, and other forms of support.
Domestic violence cases have doubled in Thailand during the quarantine period. Similar rises have been recorded in countries across the region including Bangladesh*, Singapore and Malaysia.
During the lockdown children have been spending more time online for education, social media or entertainment and are potentially being more exposed to cyberbullying, harmful content and sexual exploitation.
A post-COVID world where girls survive coronavirus, only to be denied their rights and prevented from having opportunities, is intolerable.
In Bangladesh, April’s national impact and needs assessment compiled by a range of stakeholders including World Vision, revealed that beatings by parents or guardians had increased by 42%; that there was a 40% increase of calls to the child helpline; and that 50% of those interviewed said the safety and security of girls was an issue in the lockdown. (p.9).
Females have been disproportionately affected during coronavirus by contributing more to Unpaid caring, housework, with considerations for the affordability of childcare, as well as increased domestic abuse and being locked in homes with perpetrators. Females also hold a number of part-time and casual work roles which have been significantly reduced during coronavirus. The additional stress on households and the lack of further opportunities with some industries such as hospitality and travel being negatively affected for may years to come.
Moving forward during coronavirus and post coronavirus by looking at potential actions to address some of these issues might include:
- Address gaps in knowledge about violence against women;
- Challenging attitudes that trivialise violence against women and further perpetuate lack of trust in women’s reports of violence;
- Make sure people know what resources are available to support them if there is a domestic violence issue;
- Mobilise individuals to look out for signs of domestic abuse in others and what actions they can take to support that individual
As one of the most accessible health professionals, pharmacists need to be aware of the signs to look out for in patients or work colleagues that might indicate domestic abuse and how to start conversations without patients feeling judged or uncomfortable. Some actions from those who are experiencing abuse might include: being prevented from communicating with friends and family, controlling your movements, withholding money, being angry and blaming you, taking away our computer or phone, missing appointments, changes in make-up, changes in clothing i.e. high necked clothing, uncomfortable behaviour of one partner when next to the other.
Mentoring of the female workforce, as well as focus on upskilling and acknowledging transferable skills, will be instrumental in moving forward with careers during and post coronavirus. Options include: online training, getting your resume and cover letter updated by using online resources or professionals, utilise your network to look for mentoring and job opportunities, write a list of your transferable skills that can be used for an interview in another role examples include; dealing with a difficult colleague or customer, negotiating, your strengths and weaknesses.
Increased funding and focus from Regional leaders and governments to ensure that every girl has the opportunity to grow and develop free from violence and fear, being protected, respected and empowered. Which may look like more investment in shelters, more career support, more investment in education, more investment into phone lines and internet support and more awareness of the support available for those who might be affected.
Sexual and gender-based violence support services remain open, safe, accessible and funded for girls and women who need support.
Pharmacists experiencing abusive behaviour and violence in the workplace
Author: Kay Dunkley, Executive Officer, Pharmacists’ Support Service (Australia)

It is well-known that a large proportion of healthcare workers experience abusive behaviour and violence in the workplace, this includes members of the pharmacy profession. The type of abusive and violent encounters range from verbal threats and abuse, psychological abuse, threats or intimidating behaviours, threats with a weapon, sexual harassment and assault, physical assault and murder. Violence could be perpetrated by customers, patients, co-workers or a member of the public who enters the pharmacy with the intent to commit a criminal act.
Risk factors for violence in any workplace have been identified:
(a) face-to-face contact with clients or customers, and
(b) cash or high-value goods, including drugs of dependence on-site which may attract perpetrators of crime.
Community pharmacy fulfils both these criteria; hence pharmacists and all staff working in community pharmacies may be considered at high risk of experiencing violence within the workplace.
The implications of experiencing violence in any form in the workplace are potentially significant on a number of levels. On a personal level, pharmacists and pharmacy staff exposed to abusive behaviour and violence may experience distress, shock and trauma. This may be seen as emotional disturbance, which can include sobbing and tears, expressions of frustration and anger or a sense of numbness and unreality. Exposure to trauma at work can create a sense of anxiety and fear in individuals when in the pharmacy workplace and a reluctance to return to work. In some instances, exposure to trauma will lead to Post Traumatic Stress Disorder (PTSD) with significant morbidity for the pharmacist or pharmacy employee.
On a wider scale, a major concern is whether the incidence of violence in pharmacy has the potential to impact retention rates within the profession. Chronic exposure to violence has been linked to job dissatisfaction, stress-related illnesses and absenteeism, which may potentially exacerbate any shortages of pharmacists or pharmacy staff. The financial impact can also be significant in terms of compensation, legal costs and the costs for pharmacies to take countermeasures to ensure the safety of their staff.
During the COVID-19 pandemic, pharmacists and pharmacy staff have experienced increased levels of abuse and violence in community pharmacy. It is likely that this has been due to the fear, anxiety and frustration experienced by members of the public due to stock shortages and strict limits on the amount of medicine supplied. These limits were directives from government authorities under the emergency provisions in order to reduce panic buying which would result in inequitable access to essential medication.
Examples of the violence include:
- A pharmacist punched in the face trying to prevent hoarding of boxes of tissues.
- An individual throwing stock at a pharmacist and causing injury requiring medical attention.
- An individual who attempted to throw an item at a pharmacist, but instead hit another customer who experienced a significant injury.
- An individual threatening to spit at a member of pharmacy staff.
These examples are in addition to many pharmacists and pharmacy staff experiencing verbal abuse.
In addition, pharmacists and pharmacy staff continue to be subject to hold-ups with individuals and small groups entering pharmacies and demanding cash and drugs. As well as threatening staff with a weapon during a hold-up those present are often subject to verbal abuse and threats including swearing and offensive language.
While it is not possible to entirely eliminate this type of behaviour there are actions which can be taken to reduce the risk to those working in a pharmacy. Security measures may include the following:
- Use of security cameras.
- Employment of a security guard.
- Employment of adequate staff to reduce waiting times and discourage customers from spending long periods of time observing how the pharmacy operates.
- Employment of adequate staff to ensure that all customers are supervised and assisted promptly.
- Time-delayed access to safes where money and drugs of addiction are stored.
- Limiting levels of cash held on the premises.
- Limiting the quantity of drugs of addiction held on the premises.
- Avoid having set times when cash is removed or added to the cash registers or when cash is taken to the bank.
- Encourage use of cards rather than cash to reduce the amount of cash held on the premises.
- Having a pharmacy layout which does not have a direct route from the entrance to the dispensary or the cash register.
- Being prepared to ask a customer to leave the store when their language or behaviour is inappropriate. Repeat offenders can be banned and if necessary, an intervention order obtained.
- Request police attendance when necessary.
It is also important to ensure that pharmacy staff are well trained in communication techniques which are likely to reduce anger and aggression in a customer who is lodging a complaint. One of the key aspects is good listening skills and the ability to convey empathy. Reflective listening and acknowledging what has caused a customer to make a complaint are essential. Apologising if a customer has been inconvenienced is also essential. Offering potential solutions and advising how the situation will be managed is also important. When appropriate refer the issue to a staff member with the authority to make a decision with regard to the complaint. It is important to remain calm even if a customer is displaying anger or shouting. Avoid raising your voice and if necessary, ask the customer politely to lower their voice – for example saying something like “I cannot understand you very well when you shout, please lower your voice as I want to be able to help you.” Responding quickly to any customers who are showing signs of distress or anger is important. In addition, managing complaints away from the busy areas of the pharmacy will aid good communication and remove any “audience” that the person lodging the complaint may be seeking to appeal to. However, it is important to consider the safety of any staff member in this situation and if possible, it is best to ensure that there is a counter between an angry customer and the staff member, as well as an escape route if a customer becomes violent.
Each pharmacy can also make it quite clear to customers that abuse and violence will not be tolerated. This can be undertaken though appropriate signage and communication to customers. Many of FIP member organisations have issued advice and guidance for pharmacy teams, we are collating a list of these on our COVID webpage. Staff in a pharmacy can set the tone of behaviour in the way they speak to each other and the way they speak to customers. As mentioned above, abuse and violence can also be perpetrated by a staff member towards another staff member. This will always breach occupational health and safety requirements and any bullying or harassment must be dealt with promptly by a senior member of staff including the pharmacy manager and/or the pharmacy owner. Every pharmacy should have a policy in relation to bullying and harassment which is implemented, if required.
After any incident of abuse, bad behaviour or violence all staff members involved should be provided with an opportunity to debrief. Generally, this can be undertaken with colleagues or a support service such as the Pharmacists’ Support Service (PSS) in Australia. In Australia, the PSS offers support and a listening ear over the phone by pharmacists who are trained volunteers. Some staff may wish to consult their doctor or psychologist for counselling and support if they feel very impacted by the event. Debriefing should be optional as not all staff members will want it or require it. Each individual will have difference degrees of tolerance to poor behaviour by others in the workplace and different coping mechanisms.
In conclusion, pharmacists and pharmacy staff may be exposed to abuse and violence in their workplaces. This is never acceptable and as a profession we must continue to call out this behaviour and advocate to be treated courteously and with respect. Pharmacists and pharmacy staff have a right to feel safe in their workplaces.
Further reading
Gregory M. Peterson, Sean Im Tan, Shane L. Jackson, Mark Naunton. Violence in community pharmacy in Australia: incidence and implications Int J Clin Pharm (2011) 33:264–272
Pharmacists’ Support Service www.supportforpharmacists.org.au
A collection of women’s experiences with regards to sexual harassment
Author: Carlene Ngoma, FIP Global Lead for FIP Development Goal 10 Equity & equality (Australia)

When we discuss sexual harassment, it is often described as unwelcome and inappropriate behaviour. It can be difficult to define and describe and can ultimately lead to a person feeling very lonely in their situation and it can be difficult to prove how someone makes you feel…is sexual harassment repeated incidences with escalations or can it be one single incident that made you feel very uncomfortable and avoid a person? This is what can make it hard to define…also the longer it occurs the more a victim might justify a situation or blame themselves. They may try to rationalize behavior in the beginning and this may lead to escalation which may make a victim feel like they have contributed to the situation. How do you gain the confidence to speak to a perpetrator and tell them they make you feel uncomfortable and that their actions are inappropriate. How do you then handle the perpetrator trying to blame everything on you and potentially ‘bully’ you for calling them out?
In many cases this might have led a person to quit, change their work location or hours and all as a response to someone else’s inappropriate actions that might be to your detriment. But sometimes this can seem like the quickest and easiest solution but you might not be their only victim and you might have removed yourself as victim, but not done anything to hold the person accountable, and where do your responsibilities end?
The impact of being taken advantage of, of being in fear and intimidated as well as humiliated can have significant impacts on your mental health. To describe the situation and how they made you feel and how they potentially continue to impact your life can be very difficult and not a situation you hope to be in. Talking to someone can help…someone who might have had similar experiences, someone who takes your situation seriously and can make a positive impact and help you as you navigate through the process – whether you decide to confront a perpetrator, report it to your boss or try to avoid the person; each of these situations has consequences and can impact on your mental health.
Most people try not to talk about it due to stigma and blame. Who you confide in and their response is very important. Be careful of questions such as ‘when did this first happen or why did you let this go on for so long’. Victim blaming only further victimizes someone who has gone through a challenging experience and can hinder their healing process as well as fail to rectify the situation by not holding the perpetrator accountable.
Intimidation is another way that people try to control victims and make them feel like they will not be believed if they try to share their experiences. There can be a significant difference in power both professionally, physically and tenure with a company that can make victims second guess whether they should report the situation.
As mentioned in the article sexual harassment in pharmacy in the Australian pharmacist magazine December 2019/January 2020 ‘the right support and advice through the process, and holding the perpetrator accountable, can lead to confidence, empowerment and prevention’.
Feeling safe to share your story with employers is important and employers should ensure they have the appropriate standard operating procedures and policies in place to deal with a complaint and be prepared and familiar with the process. It is your responsibility to make employees feel as though they can work in a safe environment and hold people accountable those who exploit others. Employers can continue to cause harm if they try to justify inappropriate behavior, do not take the accusations seriously, defend a person or fail to make a person responsible.
It is a situation that has stigma associated with it towards the victim that can prevent them from reporting the situation and fear of the consequences on their employment, career, opportunities, or even by being bullied and misunderstood by colleagues and not having support.
Not everyone feels comfortable ‘making waves’ and being someone who challenges a person, a culture or an environment. Sometimes others have already made complaints and been ignored. In this situation it would be best to speak to the individuals who have similar experiences to you and gather information. You may feel the company is not supportive of you and you might find you need legal or other advice or support and then also hold the company accountable for their lack of action and response to the situation.
Ultimately, it is the management’s responsibility to uphold a safe working environment. It is the employers’ responsibility to make employees feel like they can report inappropriate behavior safely and without further penalty in a professional manner.
A perpetrator can start their victimizing slowly and subtly by grooming or manipulating a person and this can also make a person try to justify the behavior or feel as though they are somehow to blame. But perpetrators can be skilled at these actions not only to victimize the person by the initial inappropriate actions but also by continuing to control the person and the narrative to suit their needs.
It is important to keep note: dates, locations, what was said and done and how it made you feel in case of further action or to make it easier for employers to hold perpetrators accountable with specific incidences. There is also a statute of limitations on sexual harassment cases and that will vary between countries and it is important that you are aware of your own country’s statute of limitations to ensure that you can seek the right kind of justice.
It is also recommended that you give a clear message to the perpetrator that the behavior is unacceptable. You need to not justify actions or excuse them and be specific and firm in your discussion. Role plays might help in this situation with trusted confidants or calling a pharmacy support service and gaining their advice for your specific situation or speaking to your professional indemnity company for their advice.
It is important to know you are not alone and there are many resources available to you. You are not to blame. Perpetrators can be skilled at grooming and exploitation and it is important to talk to a trusted confidant, gain confidences in directly speaking to perpetrator about inappropriate behavior after utilizing resources, record details of offences and employers to have the right policies and procedures in place to handle these situations to ensure that perpetrators cannot exploit others and that victims can feel safe at work.
Maternity and paternity experiences… can you relate?
Author: Carlene Ngoma, FIP Global Lead for FIP Development Goal 10 Equity & equality (Australia)

My recent experience of becoming a mother for the first time has compelled me to have discussions with other mothers and find out about their stories and experiences with regards to workforce attitudes towards maternity & parental leave. Maternity for an employee brings about many questions, including “Will my training and promotion goals be delayed?”, “Will the way my colleagues and boss interact change?”, “Will more or less be expected of me?”, and “When should I tell my work?”.
For employers, they too will have many questions: “Will my employee require much sick leave?”, “Will I need to hire a replacement during the maternity or paternity leave?”, “Am I putting too much pressure on my staff member?”, “What is the company’s culture and guidelines on maternity?" – not to mention the additional paperwork!
When you find out that you are expecting a baby, there are so many questions and things to plan for: nursery, change to your family dynamics, priorities changing, fatigue, and then workplace politics, ethical and legal matters regarding maternity leave.
Most women worry when to tell their employers about their pregnancy, as they may potentially be confronted with two potentially negative results; being the employer who removes many tasks to accommodate the potential changes you might experience due to your pregnancy without any discussion or input from yourself; or the employer who believes you should work harder to ‘earn your maternity leave’.
Through my discussions with many mothers, these two experiences are unfortunately extremely common. They also found that they had to have immediate answers for their employer: “When will you be taking maternity leave?”, “For how long?” and “Will you be coming back to work at all?”.
For many mothers, especially first-time mothers, these are questions that they may not have answers to; they themselves will be waiting to see how their pregnancy progresses and they too have no concrete answers or expectations. Even if they did… their baby might have other plans!
Mothers are subject to many discriminatory practices from employers and managers. For example, when they make it known that they will be taking maternity leave they have been asked “Is the training necessary as you will only be here for 3 more months?”, or when they ask if promotions are still a consideration during these pre-natal months, they are informed ‘off the record’ that usually they are not.
Employers have to consider travel expectation with a pregnant mother, in some instances pregnant women have been expected to travel up to and in their eighth month of pregnancy, in this situation individuals have handled it in different ways. These kinds of expectations can lead a staff member to consider a few options:
- To take sick leave and avoid the uncomfortable conversation, pregnant mums might not want the additional stress and have to think of their babies and their energy levels which are usually declining also
- Talk to human recourses, this brings the situation to the company’s attention and means someone else can intervene, however company cultures and expectations spoken and unspoken remain uniform between departments
- I heard of one pregnant woman who told their employer they would travel if their husband and specialist could go too as there was no way to be sure what could happen. Not everything is predictable or can be planned in pregnancy and if things go wrong, they can be sudden and urgent attention and care is needed with your family by your side and your trusted specialist and the opportunity to have the birth go as you had hoped.
Recently, I was informed by an acquaintance about how badly she was treated by her company during her pregnancy, leading her to quit and forego maternity leave. She spoke to a lawyer, but there was a short statute of limitations and she did not want to be put under that much pressure during the late stages of her pregnancy. A high burden of proof, low potential rewards and all the effort required by her to hold the company accountable served to ensure that such situations end up in the favour of some employers who create difficult workplaces.
Partners of pregnant women can also be affected by poor culture within organisations when it comes to parental leave. A male colleague recently had an experience where he told his colleagues that he and his wife were planning on having a baby; when he went for a more senior role, they asked if he was able to do it with the changes about to happen in his family. Unfortunately, many people have had one of these experiences and it can be at any part of the pregnancy journey or upon returning to work.
It is important for expectant mums to be as prepared as possible when telling their company about their pregnancy; it is important from a health and safety perspective, but also having the discussion early on about travel, about how much time you might want to take off before the baby comes, any jobs you might not be able to do i.e., that require heavy lifting.
It is important for employers to have an open mind and be aware that the expectant mother do not have all the answers, energy levels will vary, some jobs might not be able to be undertaken, and that the expectant mother still may have career aspirations and goals they would like to be working towards.
Employers need to have a transitional process in place for mothers who return to work to help with the readjustment. Having standard operating procedures in place for bullying and how to handle it; in practice there is still blaming of the victim without taking accountability of company culture or rights to a safe working environment. It is excellent to have a policy of inclusion and re-integration to the workforce, but this services no purpose if the organisation just blindly believes that this happens without ongoing effort to maintain it.
There are many ethical, legal and political considerations with regards to maternity and this leads many women to experience significant stress at a time when they should be excited. It can lead to workplaces being held legally accountable or ethically being questioned as to how they treated or enabled a staff member to be treated during their pregnancy and early parenthood.
Having standard operating procedures, guidelines and processes in place for maternity can create some much-needed structure around the process. Having the right processes, the right documentation and open frequent discussions would be a great start to resolve some of these situations.
I would advise keeping records of dates and witnesses to discussions or emails that have been shared between yourselves and your employers for your reference; I would advise looking at statute of limitations and receiving any legal advice regarding your situation as well as speaking to other colleagues who might be experiencing a similar situation to you. Speaking to colleagues is an important way to gauge the culture of your employer with regards to gender equality and parental leave. There are still notable wage disparities between males and females in the workplace and women being of child-bearing age, taking time off for maternity leave and coming back to work with young children can affect wage and career progression.
A good culture could prevent losses from companies in sick leave and legal costs as well as cost to reputation. To believe in 2021 that we still have such challenging experiences during maternity as well as feeling the need to be anonymous and not own our stories says that there is still much work to be done in this area and to make progress for the next generation.
Author: Elizabeth Ridgway, FIP-EquityRx Programme Coordinator (USA)

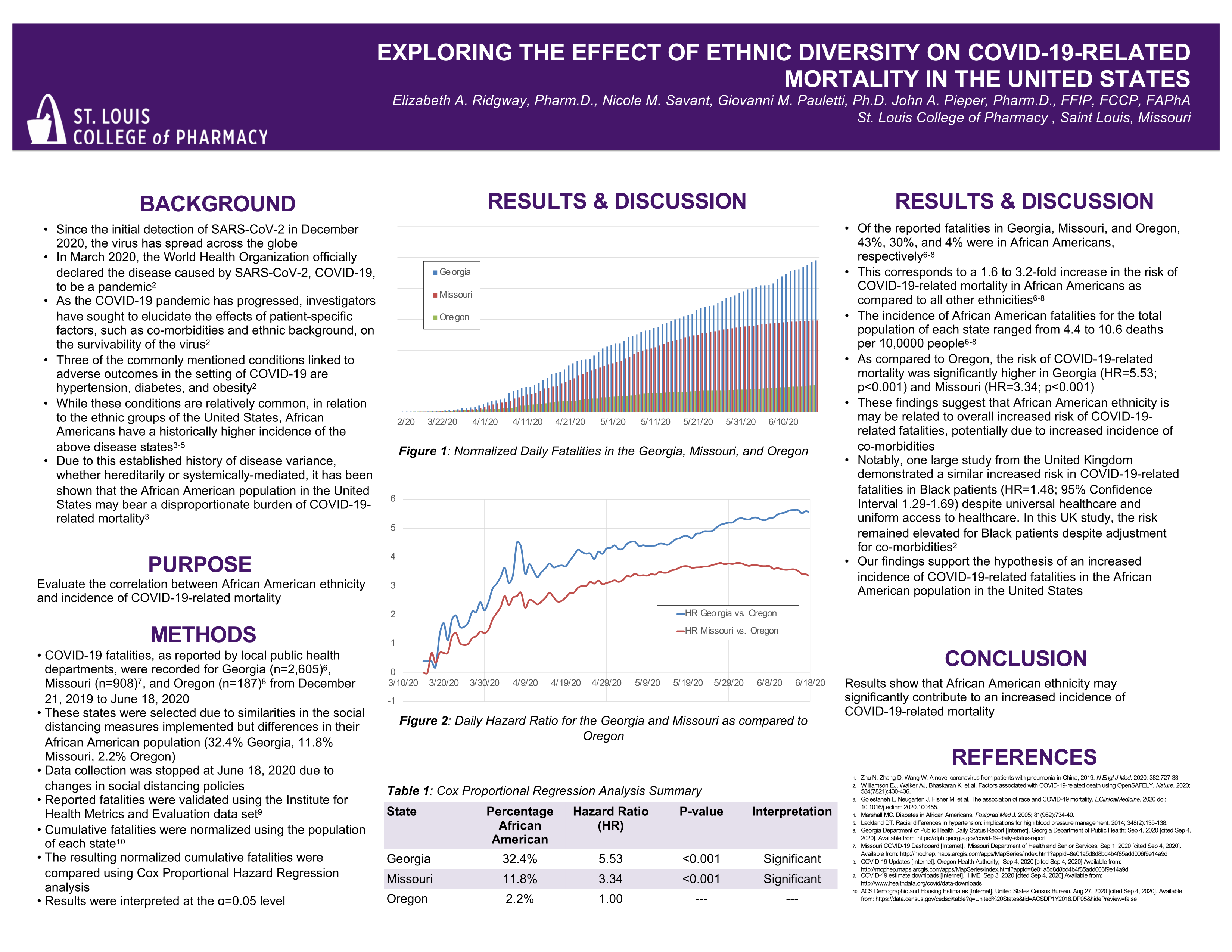
Presented at the International Pharmaceutical Federation’s 2020 World Congress, the following abstract sought to quantify the disproportionate impact that the coronavirus disease 2019, COVID-19, pandemic has had on African Americans throughout the United States. The authors effectively demonstrated that either due to genetic predisposition, underlying co-morbidities, systemically mediated healthcare inequities, or a combination of the above, African Americans are at a 1.6 to 3.2-fold increase in the risk of COVID-19-related mortality as compared to all other ethnicities.
Modelling Pandemics: Exploring the Effect of Ethnic Diversity on Mortality in the United States
Elizabeth A. Ridgway, Pharm.D., Nicole Savant, Pharm.D. Candidate 2021, Giovanni Pauletti, Ph.D., and John A. Pieper, Pharm.D., FFIP, FCCP, FAPhA
St. Louis College of Pharmacy at the University of Health Sciences and Pharmacy in St. Louis
St. Louis, Missouri, United States
Background: Since the initial detection of SARS-CoV-2 in December 2020, the virus has spread across the globe. In March 2020, the World Health Organization officially declared the disease caused by SARS-CoV-2, COVID-19, to be a pandemic.2 As the COVID-19 pandemic has progressed, investigators have sought to elucidate the effects of patient-specific factors, such as co-morbidities and ethnic background, on the survivability of the virus.2,3 Three of the commonly mentioned conditions linked to adverse outcomes in the setting of COVID-19 are hypertension, diabetes, and obesity.3 While these conditions are relatively common, in relation to the ethnic groups of the United States, African Americans have a historically higher incidence of the above disease states.3-6 Due to this established history of disease variance, whether hereditarily or systemically-mediated, it has been shown that the African American population in the United States may bear a disproportionate burden of COVID-19-related mortality.3
Purpose: Evaluate the correlation between African American ethnicity and the incidence of COVID-19-related mortality.
Method: COVID-19 fatalities, as reported by local public health departments, were recorded for Georgia (n=2,605)7, Missouri (n=908)8, and Oregon (n=187)9 from December 21, 2019 to June 18, 2020. These states were selected due to similarities in the social distancing measures implemented, but differences in their African American population (32.4% Georgia, 11.8% Missouri, 2.2% Oregon). Data collection was stopped at June 18, 2020 due to changes in social distancing policies. Reported fatalities were validated using the Institute for Health Metrics and Evaluation data set10 and the COVID Tracking Project. Cumulative fatalities were normalized using the population of each state.11 The resulting normalized cumulative fatalities were compared using Cox Proportional Hazard Regression analysis. Results were interpreted at the α=0.05 level.
Results and Discussion: Of the reported fatalities in Georgia, Missouri, and Oregon, 43%, 30%, and 4% were in African Americans, respectively.7-9 This corresponds to a 1.6 to 3.2-fold increase in the risk of COVID-19-related mortality in African Americans as compared to all other ethnicities.7-9 The incidence of African American fatalities for the total population of each state ranged from 4.4 to 10.6 deaths per 10,0000 people.7-9 As compared to Oregon, the risk of COVID-19-related mortality was significantly higher in Georgia (HR=5.53; p<0.001) and Missouri (HR=3.34; p<0.001). These findings suggest that African American ethnicity may be related to overall increased risk of COVID-19-related fatalities, potentially due to increased incidence of co-morbidities. Notably, one large study from the United Kingdom demonstrated a similar increased risk in COVID-19-related fatalities in Black patients (HR=1.48; 95% Confidence Interval 1.29-1.69) despite universal healthcare and uniform access to healthcare. In this UK study, the risk remained elevated for Black patients despite adjustment for co-morbidities.2 Our findings support the hypothesis of an increased incidence of COVID-19-related fatalities in the African American population in the United States.
Conclusion: Preliminary results show that African American ethnicity may contribute to an increased incidence of mortality.
References:
- Ridgway E, Savant N, Pauletti G, Pieper J. Exploring the effect of ethnic diversity on mortality in the United States of America. Pharmacy Education. 2020: 20(3): 71-72. (Abstract)
- Zhu N, Zhang D, Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727‐33.
- Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020; 584(7821):430-436.
- Golestaneh L, Neugarten J, Fisher M, et al. The association of race and COVID-19 mortality. EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100455.
- Marshall MC. Diabetes in African Americans. Postgrad Med J. 2005; 81(962):734-40.
- Lackland DT. Racial differences in hypertension: implications for high blood pressure management. 2014; 348(2):135-138.
- Georgia Department of Public Health Daily Status Report [Internet]. Georgia Department of Public Health; Sep 4, 2020 [cited Sep 4, 2020]. Available from: https://dph.georgia.gov/covid-19-daily-status-report
- Missouri COVID-19 Dashboard [Internet]. Missouri Department of Health and Senior Services. Sep 1, 2020 [cited Sep 4, 2020]. Available from: http://mophep.maps.arcgis.com/apps/MapSeries/index.html?appid=8e01a5d8d8bd4b4f85add006f9e14a9d
- COVID-19 Updates [Internet]. Oregon Health Authority; Sep 4, 2020 [cited Sep 4, 2020] Available from: http://mophep.maps.arcgis.com/apps/MapSeries/index.html?appid=8e01a5d8d8bd4b4f85add006f9e14a9d
- COVID-19 estimate downloads [Internet]. IHME; Sep 3, 2020 [cited Sep 4, 2020] Available from: http://www.healthdata.org/covid/data-downloads
- ACS Demographic and Housing Estimates [Internet]. United States Census Bureau. Aug 27, 2020 [cited Sep 4, 2020]. Available from: https://data.census.gov/cedsci/table?q=United%20States&tid=ACSDP1Y2018.DP05&hidePreview=false
The Unforeseen Impact of the United States Prioritizing Specific Populations During the Vaccine Rollout
Authors: Elizabeth Ridgway, Pharm.D. with contributions from Kim Hoff, Pharm.D., BCPS, BCACP

Over the past few months, I have been honoured to administer the COVID-19 vaccine in facilities throughout the state of Missouri, United States of America. This experience has been truly rewarding, but it has also opened my eyes to the systemically mediated healthcare inequities that seem to have dominated the rollout of the COVID-19 vaccine. In Missouri, the vaccine rollout has already occurred in several phases which prioritize specific populations. The first phases sought to ensure that healthcare providers, essential workers, residents of long-term care facilities, elderly patients, and individuals with comorbidities received the first doses of the vaccine. The complicated “phased” design of the vaccine rollout and the reliance on contracts with specific healthcare providers to distribute the vaccine have exacerbated long standing health inequities.
The “phased” approach to the rollout of the COVID-19 vaccine sought to prioritize high-risk individuals, however it inadvertently caused several health inequities providing an opportunity for lessons to be learned. Initially, the vaccine was rolled out in long-term care facilities and hospitals, however almost immediately there were reports of wealthy donors and administrators receiving the vaccine prior to facility residents and medical staff in direct patient care roles. As the vaccine has been rolled out to the next phases, patients have been required to “hunt” for the vaccine, a process often requiring internet access and technological prowess, large amounts of time, some level of familial or personal connections to hospital, pharmacy, long-term care facility, or local health department staff, and finally reliable access to transportation. The sad reality for patients with mental disabilities, those living “paycheck to paycheck”, and those without reliable access to transportation is that they are likely to wait much longer to receive the vaccine simply because the system doesn’t appear to have been designed with them in mind. Furthermore, the lack of communication and constant changes in policies and regulations with regards to the vaccine rollout has had a disparate impact on disadvantaged patient populations due to a lack of up-to-date information and limited access to health care professionals.
In Missouri, the use of contracts allowing specific pharmacies and hospitals to vaccinate specific patient populations limits the provision of equitable patient care and is a constant source of confusion. These contracts mean that one location may be able to vaccinate a patient based on where they live, another may be able to vaccinate a patient due to their work duties, and another may be able to vaccinate a patient due to their age. This scheme is confusing both to the public and to healthcare providers. The inability of pharmacies, which are already ingrained in communities around the state, to vaccinate during all phases of the vaccine rollout has disproportionately affected many traditionally underserved communities as patients in these areas are less likely to know where else they can go to get the vaccine. Additionally, COVID-19 vaccines are often distributed into areas that are unable to fully utilize the available doses, leaving a significant number of left-over doses that may be difficult to utilize prior to the expiration date while still ensuring company and state policies and procedures are upheld. Thus, “approved” patients are asked to travel from the cities to rural areas to avoid waste in a time pressured situation. For patients with limited access to transportation or who are unable to afford to leave work, these situations further limit their access to the vaccine. This common situation also means that pharmacists are unable to vaccinate their local communities as they are expected to first reach out to those patients who have been added to a company-approved list.
While over the past few months I have witnessed first-hand a number of health inequities, I have also been able to help some of Missouri’s most vulnerable patients. Despite its problems, I believe that the rollout of the COVID-19 vaccine has been overarchingly successful and I hope that, as policies continue to evolve, we are better able to address the needs of all communities and ensure equitable access to care.
In our
2019 FIP-EquityRx Collection, we presented examples of transformative policies & initiatives from around the globe; a national case example from Pakistan was featured. More than a year onwards, those efforts in Pakistan have blossomed into a national equity hub. The authors report below.
Authors: Nadia Bukhari, Equity Pakistan Director (UK) and FIP Global Lead for FIP Development Goal 10 Equity & equality; Madeeha Malik, Equity Pakistan Director (Pakistan)

On February 25, 2021 Equity Pakistan, the Gender Equity hub for the pharmaceutical workforce in Pakistan, was launched in Islamabad, Pakistan. The hub is a collaboration between UCL School of Pharmacy (UK), & Hamdard Institute of Pharmaceutical Sciences Islamabad (Pakistan); and is supported by FIP, The International Pharmaceutical Federation (NL), the British Council (UK) and doctHERs (Pakistan).
Background
According to World Economic Forum report 2018, Pakistan is ranked 148 out of 149 in gender inequality status. The number of managerial positions occupied by female workforce is low as compared to other developed countries. Women currently comprise more than 70% in the academic medicine workforce, yet make up a mere 3% of the legislators and senior officials in the country. The Employment-to-Population Ratio (EPR) is 20% for female workers and 64% for male workers. Moreover, Pakistan’s current labour underutilization rate for women workers is currently 80%. The barriers for female labour force participation include educational attainment, local customs and social norms, availability of work-family reconciliation measures (including part-time work for women), lack of affordable transport and childcare, workplace harassment and discrimination, and work-family balance. Pakistani GDP could increase by nearly one-third if the female labour force participation rates match those of males.
Taking all these factors into consideration, it is increasingly necessary to provide a platform to identify and provide solutions for these national workforce issues. The Pakistan Gender Equity Hub “Equity Pakistan” is being established to focus on both gender equality issues (decent working conditions, for example) and educational equity in Pakistani civil society. From a professional perspective, the Pakistan Gender Equity Hub will be a source for generating evidence-based data on the healthcare workforce in Pakistan with a particular focus on the pharmaceutical workforce. Moreover, the Hub will lead the implementation of recommendations generated by the data and directly influence policy formation. The Hub will aim to accelerate large-scale gender-transformative policy change to address gender inequities in Pakistan. This, in turn, will significantly influence progression towards achievement of the FIP Development Goal 10 (FIP DG 10 https://www.fip.org/fip-development-goals) and the UN Sustainable Development Goals (SDGs), as envisioned in the Working for Health five-year action plan (2017 – 2021). The Pakistan Gender Equity Hub will provide a base for transformative actions stemming from the FIP global policy and the WHO Gender Hub
‘Equity Pakistan’ is comprised of multidisciplinary members including policymakers, practitioners, academia, civil society, professional bodies and researchers from diverse set of stakeholders and partners.
Vision
Equity Pakistan addresses gender inequities and develop transformative gender and diversity policies for the pharmaceutical workforce in Pakistan. It forms a national focus for gender-balanced workforce transformation and acts as a direct national link with the global equity programmes from FIP and WHO Human Resources for Health. In this way, Equity Pakistan will transform equity and equality for professional women and advocate for the critical importance of women’s participation in the pharmaceutical workforce of Pakistan.
Aim
Equity Pakistan will create clear evidence-based strategies for addressing gender and diversity inequalities in pharmaceutical workforce development in Pakistan for continued education and training and career progression opportunities.
Strategic Goals
Equity Pakistan will provide a comprehensive summary of the current evidence base on gender equity and to generate and report updated findings via systematic review, meta-analysis. It will investigate the gender equity issues of the healthcare workforce in pharmacy via a needs-based assessment of the current gender equity situation in Pakistan using validated tools. One goal will be to develop a national framework for addressing the issues identified from these assessments.
In order to increase awareness of women’s rights and national cross-sectorial women empowerment initiatives, Equity Pakistan will work with professionals, employers and unions to eliminate discriminatory behaviours & attitudes at workplace.
The Equity hub objectives will be aligned with national and international policy directions, and the Hub will be a collaborator with relevant stakeholders for monitoring and evaluation of Hub objectives in terms of National priorities and goals.
The purpose of the Equity Hub is to achieve fair solutions to the gender equity in the pharmaceutical workforce challenge and will therefore be aligned with global trends of issues concerning equity. Due to the need for global perspectives, the Equity Hub has direct support from the British Council in Pakistan who have agreed to provide resource with respect to research activities, as well as the British High Commission in Pakistan.
In addition, The Hub has the full support of the International Pharmaceutical Federation (FIP) and will link into the WHO gender equity hub providing linkage with global issues surrounding gender equity in healthcare and thus providing a platform for long-term academic interest.
General References:
Young Women in Pakistan – Status Report 2020. Empowering young women key to Pakistan’s sustainable social and economic development. UN Women July 2020. https://asiapacific.unwomen.org/en/digital-library/publications/2020/11/young-women-in-pakistan-status-report-2020#view Accessed March 20231
FIP Development Goals 2020. https://www.fip.org/fip-development-goals

Women in science and education at the forefront of the fight against COVID-19 by FIPWiSE
Authors: Nilhan Uzman, FIP Lead for Education Policy and Implementation, Programme Lead for FIPWiSE (The Netherlands) & Anyango Esther Adhiambo, FIPWiSE Remote Volunteer (Kenya)
1. What is FIPWiSE?
Last year, before the COVID-19 pandemic changed our lives, the FIPWiSE (Women in Science and Education) initiative was launched on February 11th 2020 (United Nations’ International Day of Women and Girls in Science) to champion women in pharmaceutical sciences and pharmacy education.
The FIPWiSE initiative aims to engage, empower and enable women in pharmacy education and pharmaceutical science to achieve their ambitions and to attract young women and students in these fields. It aligns with FIP’s commitment to Equality and Equity, and underpins FIP Development Goal 10.
On February 11th 2021, FIPWiSE celebrated its first anniversary and you may read FIPWiSE 2020 activity report here. Achieving gender equity and empowering women while leaving no one behind is not a solo sport. We therefore recognise and take this opportunity to thank all FIPWiSE team members, supporters, and partners.
Watch the “FIPWiSE Words” launch video and learn about FIPWiSE’s vision, mission and priority advocacy areas here.
2. FIPWiSE fighting against COVID-19
2.1 FIPWiSE Words video series
The outbreak of the COVID-19 pandemic has clearly demonstrated the critical role of women educators and researchers in different stages of the fight against COVID-19, from ensuring the continuity of the education amongst unprecedented disruptions to advancing the knowledge on the virus, to developing techniques for testing, and finally to creating the vaccine against the virus.1
During 2020, the FIPWiSE words video series became the voice of women in pharmaceutical sciences and pharmacy education to showcase the breadth and depth of their talent in the fight against the pandemic. Below you can find the FIPWiSE words series from 2020:
Dalal Hammoudi Halat: How women leaders in pharmaceutical sciences are combatting the COVID-19 pandemic–
Dr. Bahijja Raimi-Abraham: Women shaping pharmaceutical sciences
Dalia Bajis: Resilience in Academia and Mental Health
Erem Bilensoy: What has COVID-19 taught women in pharmaceutical sciences?
2.2 FIPWiSE digital events
At the same time, the COVID-19 pandemic also had a significant negative impact on women in science and education, particularly affecting those at the early stages of their career, and thus contributing to widening the existing gender gap, and revealing the gender disparities in the system, which need to be addressed by new policies, initiatives and mechanisms to support.1
FIPWiSE delivered the “COVID-19: Women front and center” web panel alongside FIP’s “Responding to the pandemic together” digital event series, where FIPWiSE members discussed challenges women face during the pandemic, emphasized the critical role of women in resolving this crisis and the roles for pharmacists and pharmacy workers to empower women in the communities to support pharmacy’s response to the pandemic. Below you can find the list of speakers and you can watch the web panel here.
Dr. Mariam El Boakye-Gyasi- Senior Lecturer, Academic Capacity Lead, FIPWiSE member (Ghana)
Dr. Ecehan Balta, Senior Advisor to President, TPA, FIPWiSE member (Turkey)
Assoc. Prof. Rajani Shakya, Head, Kathmandu University, AIM Advisory Committee member; FIPWiSE member (Nepal)
Anyango Esther, Intern, Hospital Pharmacist, FIPWiSE member and intern (Kenya)
Science, education and gender equity are vital for the achievement of the internationally agreed development goals, including the 2030 Agenda for Sustainable Development.1 Women are powerful agents of change, and the benefits and effectiveness of equitable representation in leadership and decision-making are evident. To discuss the under-representation of women in the decision-making process, FIPWiSE organised the Women’s Leadership Lab alongside the FIP Virtual 2020 Congress. We featured the following inspirational speakers:
Meltem Agduk, Gender programme coordinator at the United Nations Population Fund (Turkey)
Nadia Abdelhadi, North Africa Country Manager, Medtronic (Algeria)
Christina Chai, Head of pharmacy department, National University of Singapore (Singapore)
Leonora O’Brien, Founder & CEO, Pharmapod (Ireland)
Vibhuti Arya Amirfar, Associate Clinical Professor at St John’s University College of Pharmacy and Health Sciences, and Clinical Advisor to the New York City Department of Health and Mental Hygiene (USA)
Aya Jamal, President, International Pharmaceutical Students Federation (Sudan)
The link to the full recording of the virtual leadership lab is here.
2.3 Supporting youth in science and education alongside the pandemic
Long-standing biases and gender stereotypes are steering girls and women away from science and education related fields.1 Throughout 2020, FIPWiSE supported early career women in science and education, as well as students to support them against the COVID-19 related disruptions on education and research.
FIPWiSE has been collaborating with the FIP Young Pharmacists Group (YPG) on a mentorship program to support young professional by recognizing the gender-specific challenges young women professionals face in areas of pharmaceutical sciences and education.
FIPWiSE provided mentors from the FIPWiSE community who were linked up with mentees. The mentors are attached to the mentees for a period of 9 months, with the intention of setting goals, providing general advice, tips and strategies to navigate gender-specific challenges and helping both young female and male pharmacists and pharmaceutical scientists to keep on track of their career development. Learn more about this programme here.
FIPWiSE released a special edition newsletter featuring stories of young female professionals and pharmacy students and their adaptation to education and research alongside the COVID-19 pandemic. There was a common undertone of hope and persistence to education in all the stories. You can find the article here.
As we are in the second year of the pandemic, FIPWiSE will continue to support and empower women in pharmaceutical science and pharmacy education to ensure they reach their fullest potential in the battle against the pandemic.
References:
- United Nations. International Day of Girls and Women in Science. 2021 (Available online:
https://www.un.org/en/observances/women-and-girls-in-science-day accessed 16 March 2021)
Deeds not words: The FIPWiSE way forward in 2021 and beyond
Author: Claire Thompson, Chair of FIPWiSE (United Kingdom)

Based on all the narratives we heard and conversations we had in 2020, we defined four priority workstreams for FIPWiSE in 2021. These workstreams will support the global implementation of the FIP Development Goal 10 – Equity and Equality to address equity and diversity inequalities in pharmaceutical workforce development, continued education and training, and career progression opportunities. The priority workstreams, key deliverables and Working Group members are listed below.
1. Confidence in competence
Role modelling and raising awareness through webinars, videos, podcasts supported through the online leadership programmes.
You can listen to the 1st FIPWiSE & Fearless podcast where we featured Vibhuti Arya, FIP Workforce Development Hub lead for FIP Development Goal 10 – Equity & Equality (USA) here.
Deliverables: FIP WiSE Digital Events, FIP WiSE words video series, FIP WiSE & Fearless Podcasts, and FIP & AACP online leadership programme “Enhancing academic leadership horizons in trying times” targeting women in science and education.
2. Enabling workplaces
Breaking down the barriers and career development through an enabling environment toolkit and online workshops.
Deliverables: “Enabling workplace environments in education & science: Breaking down the barriers’’ toolkit and online workshops.
3. Support young women in pharmacy and pharmaceutical sciences
Increasing visibility of successful young women through building platforms and scholarships.
Deliverables: Interviews with young scientists and students, FIPWiSE bursary scoping, FIP YPG Mentorship Programme.
4. Implementation of the FIP Development Goal #10
Broader implementation of FIP DG #10 through contribution to WDG leads, research & data, surveys, publications.
Deliverables: EquityRx collection, Women in workforce survey, Commitment to Equity.
5. FIPWiSE Steering Committee
FIPWiSE Steering Committee is comprised of FIPWiSE working group members who will set, challenge, and/or implement the strategy for FIPWiSE, and provide updates from the Working Groups that they represent. FIPWiSE Steering Committee also ensures engagement with wider FIP Development Goal #10 aims and includes WDH FIP DG 10 Leads.
Success is never a solo sport
Achieving gender equity and empowering women, while leaving no one behind, is not a solo sport.
We want to take this opportunity to thank all our FIPWiSE working group members, supporters, and partners. FIPWiSE will be leveraging every platform, power and privilege we have to engage, enable and empower girls and women to achieve their aspirations, and create a legacy of exceptional female leadership across science and education. The tools, traits and transformations we create will provide a platform for all within our profession to be the best they can be.
If you would like to join the FIPWiSE community, contribute to our working groups or activities, please do contact us on Education@fip.org and visit our website to learn more!